Indonesia’s Battle Against Chronic Diseases

Indonesia’s battle against chronic diseases has become a pressing public health concern. The prevalence of noncommunicable diseases (NCDs) continues to rise. According to the World Health Organization (2019), chronic illnesses such as diabetes, cancer, cardiovascular disease, and chronic respiratory illnesses account for a large proportion of deaths in the country. This situation imposes considerable pressure on Indonesia’s healthcare system and the initiatives aimed at improving public health outcomes.
To address this, Indonesia has introduced several prevention and management strategies, including public health programs and healthcare training initiatives. Nevertheless, combating chronic diseases demands persistent dedication, creative solutions, and collaborative efforts from all sectors of society.
This article explores the present condition of chronic diseases in Indonesia, emphasizes essential preventative and management techniques, and investigates the obstacles encountered in addressing this escalating epidemic. By addressing these issues and empowering healthcare professionals, Indonesia can take meaningful steps toward reducing the burden of chronic diseases on its population.
Overview of Noncommunicable Diseases (NCDs) in Indonesia
1. Latest Epidemiological Data
Noncommunicable diseases (NCDs) are responsible for around 74% of all deaths worldwide. Approximately 41 million people die annually due to NCDs, with over 17 million of these deaths being premature (i.e., occurring before the age of 70).
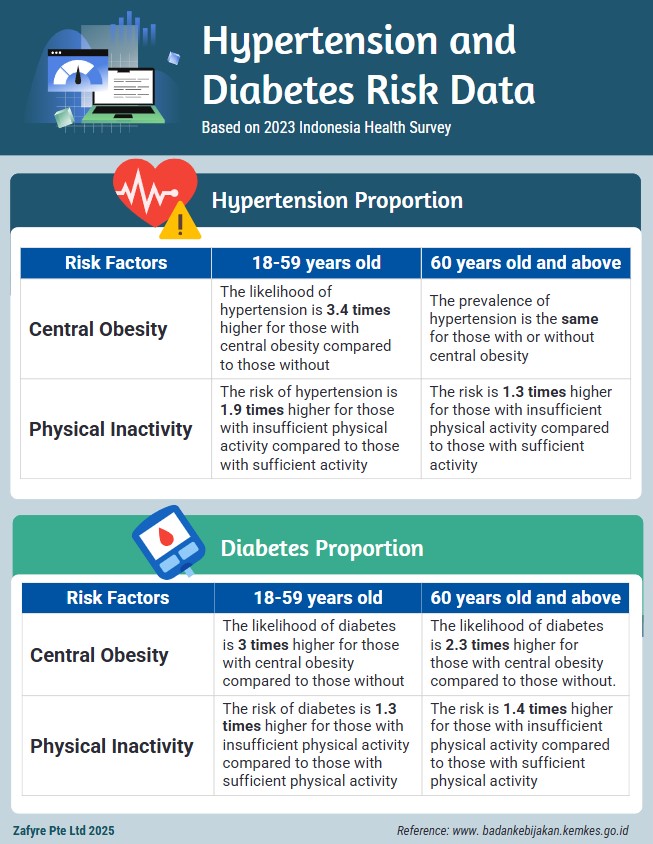
The results of the 2023 Indonesia Health Survey (SKI) indicate the continued high prevalence of hypertension (30.8%) and diabetes (11.7%) based on blood pressure measurements and blood sugar level examinations.
The survey shows that 59.1% of the causes of disabilities (vision, hearing, walking) among individuals aged 15 years and older are acquired diseases, with 53.5% of these diseases being NCDs, especially hypertension (22.2%) and diabetes (10.5%).
2. Key Risk Factors
Based on the presence of risk factors, the occurrence of hypertension and diabetes is higher in groups with central obesity or insufficient physical activity.
3. Socioeconomic Impact
Healthcare Costs: NCDs impose a heavy burden on Indonesia’s healthcare system, with significant costs associated with treatment and management . Indonesian Health Economics Association (INAHEA, 2019).
Reduced Productivity: The impact of NCDs on labour productivity is substantial, with many individuals affected by these diseases experiencing decreased work capacity and increased absenteeism (Marthias et al., 2021)
Financial Burden on Families: The financial burden of NCDs on families is immense, with many households facing catastrophic health expenditures due to the high cost of continuous medical care . This exacerbates poverty and economic strain on affected families (Marthias et al., 2021).
Prevention Strategies

1. Public Health Initiatives: Indonesia has initiated multiple public health campaigns aimed at raising awareness about the risk factors associated with noncommunicable diseases (NCDs), such as tobacco use, poor diet, and lack of physical activity.
2. Regulation and Policy: The government has enforced rules to reduce tobacco consumption, minimum smoking age, imposing higher taxes and restrictions on advertising for tobacco products.
3. Promotion of Healthy Lifestyles: There are programs in place that encourage healthy living, including guidelines for nutrition and recommendations for physical exercise.
4. Social and Cultural Influences: The government is actively addressing societal beliefs and cultural practices that obstruct efforts to prevent noncommunicable diseases (NCDs) to ensure the success of health interventions. Additionally, approaches that respect the traditions and values of local communities are being developed to encourage healthier habits.
Management Strategies

1. Integrated Care: Indonesia is working on incorporating non-communicable diseases (NCDs) into primary healthcare services to deliver comprehensive and ongoing care for patients.
2. Healthcare Infrastructure: Initiatives are underway to enhance the healthcare infrastructure to more effectively manage chronic diseases. This involves improving access to healthcare services and guaranteeing the availability of essential medications.
3. Community-Based Programs: Health programs within communities are being designed to aid in the management of chronic diseases at the local level, as reflected in the increased visits to healthcare facilities, the implementation of vaccination and screening programs, and participation in community health education (Nurjanah et al, 2024).
4. Digital Health Solutions: The government is leveraging telemedicine, mobile applications, and various digital tools to improve access to care and maintain treatment continuity.
5. Multidisciplinary Approach: Expertise from various healthcare disciplines is integrated through cross-professional collaboration to ensure holistic patient care and improve treatment outcomes.
Challenges
Despite these efforts, the country continues to face considerable challenges. These include:
1. Limited Resources
Indonesia is experiencing a lack of healthcare workers, especially specialists (Putri, 2023). Additionally, this shortage is intensified by the inadequate number of training facilities and resources available (Octavius et al., 2023).
2. Quality of Education
The standard of medical education varies significantly among different institutions. Many newly founded institutions still offer subpar education, which negatively impacts the skills of healthcare professionals (Octavius et al., 2023).
3. Coordination and Integration
A policy brief from the U.S. Agency for International Development (USAID) emphasizes that the disorganization within Indonesia’s healthcare sector obstructs the successful execution of training programs and the integration of care services. This lack of coordination among various sectors involved in healthcare delivery is considerable and creates obstacles to enhancing healthcare results (Teplitskaya et al., 2021).
4. Data Collection and Monitoring
Effective data gathering and monitoring frameworks are crucial for assessing the success of training initiatives and healthcare interventions. Nevertheless, Indonesia’s existing systems fall short, complicating efforts to monitor progress and pinpoint areas needing enhancement (Mustika et al., 2019).
5. Economic Burden
Both individuals and the broader economy are impacted by high healthcare costs and diminished productivity due to chronic illnesses (Marthias et al., 2021). According to Endarti et al. (2024), a significant number of patients face financial burdens from out-of-pocket costs for expensive medications that health insurance does not cover.
6. Patient Perspective
Patients encounter numerous obstacles in obtaining healthcare for chronic diseases, including stigma, financial challenges, and accessibility issues (Malini et al., 2023).
Key Studies and Reports Highlighting Strategic Initiatives

1. Medical Education in Indonesia (Mustika et al., 2019)
The evolution of medical education in Indonesia highlights the journey of medical education from the Dutch colonial period to the present day. The implementation of the competency-based curriculum (CBC) and the dramatic growth of medical schools have raised concerns about the quality of medical education nationwide. Enactment of laws on medical education, accreditation of medical programs, faculty development, and the national competency-based examination have been instituted to improve the quality of medical education.
2. Policy-in-Practice Case Study (United Nations Population Fund, 2022)
The Strategic Plan of the Ministry of Health 2015–2019 focuses on addressing the healthcare needs of an aging population. The plan emphasizes the importance of healthcare training to address the needs of an increasing number of older people living with chronic diseases. It focuses on providing holistic and person-centered care across preventive, promotive, curative, rehabilitative, specialist, palliative, and long-term care services.
3. Youth Employment in Health (United States Agency for International Development, 2020)
The case study highlights opportunities to increase youth employment in health in Indonesia. It emphasizes the importance of technical and vocational education and training (TVET) institutions in building the future health workforce. The study also stresses supporting youth contributions to the healthcare sector. Additionally, it calls for creating an enabling environment for their development.
Importance of Healthcare Training in the Prevention and Management of Chronic Diseases
1. Early Detection and Diagnosis
Adequate training enables healthcare professionals to identify and diagnose chronic illnesses at an early stage. Early recognition is vital for effective management and treatment strategies.
2. Patient Education
Educated healthcare providers instruct patients on making lifestyle modifications and managing their own health. Such approaches can help prevent or slow down the advancement of chronic conditions.
3. Community Involvement
Educational programs incorporate community outreach initiatives, which help increase awareness and encourage preventive actions at the local level.
4. Multidisciplinary Approach
Thorough training promotes a collaborative approach where diverse healthcare professionals team up to deliver comprehensive care.
5. Enhanced Treatment Outcomes
Ongoing training ensures that healthcare professionals remain informed about the most current treatment guidelines, which results in improved patient outcomes.
Future Directions for Indonesia’s Battle Against Chronic Diseases
As chronic diseases continue to rise, there is a need for innovative and comprehensive strategies to address their growing impact. Future directions in this battle focus on expanding partnerships, enhancing data systems, adopting digital health technologies, advocating for robust healthcare policies, and global comparisons. These measures aim to improve access to care, streamline disease management, and foster sustainable healthcare solutions for the nation.

1. Expanding Public-Private Partnerships
Collaborations like the Novo Nordisk-Bio Farma partnership for insulin production have demonstrated significant potential in addressing specific chronic diseases, such as diabetes. In July 2024, Novo Nordisk, a Danish pharmaceutical company, partnered with Indonesia’s state-owned Bio Farma to produce insulin locally, as reported by Reuters.
This initiative, which aims to combat diabetes—a condition affecting over 19 million Indonesians—not only ensures better access to essential medicines but also strengthens the healthcare system’s ability to manage chronic diseases effectively. Expanding similar partnerships across various sectors can further improve access to medicines, technology, and expertise, benefiting more patients and enhancing healthcare delivery nationwide.
2. Enhancing Data Systems
Developing robust data systems for monitoring, evaluating, and optimizing healthcare strategies is crucial. Reliable data helps identify trends, measure the success of interventions, and inform evidence-based policies, ensuring targeted and effective responses to chronic disease management.
3. Scaling Digital Health
Adopting telemedicine and mobile health tools can bridge the gap in access to healthcare, especially for remote or underserved areas. Scaling digital health solutions allows patients to receive timely consultations, manage their conditions more effectively, and maintain continuity of care.
In Indonesia, several leading telemedicine platforms, such as Halodoc, Alodokter, and Good Doctor, have successfully attracted millions of users. These platforms offer a wide range of services, from consultations with general practitioners and specialists to medication delivery and other healthcare services. Advanced features like artificial intelligence (AI) are also being integrated into telemedicine platforms to assist with disease diagnosis and provide more personalized treatment recommendations.
In addition, applications like ‘SehatQ‘ provide telemedicine services for various health conditions, including mental health, while ‘Homecare24‘ offers home care services, including nursing and physiotherapy. These platforms demonstrate the growing diversification of telemedicine services, increasingly tailored to meet the specific needs of Indonesian communities (Sitanggang et al, 2024). Read more about telemedicine in Indonesia by checking our previous article here.
4. Policy Advocacy
Advocating for sustainable healthcare policies that address chronic diseases is essential for long-term success. This involves ensuring that policies prioritize prevention, treatment, and support systems for patients while allocating adequate resources to strengthen the healthcare system.
A notable example is the recent Smoking Age Regulation, based on Government Regulation (PP) Number 28 of 2024 under Law No. 17 of 2023 on Health. In July 2024, Indonesia raised the minimum smoking age from 18 to 21 and introduced new health regulations to curb smoking. These measures reflect the country’s commitment to reducing the incidence of chronic diseases linked to smoking and promoting a healthier population (Widianto,2024).
5. Global Comparisons
Learning from other country’s best practices can provide valuable insights into what strategies have been successful in managing chronic diseases. By adapting these lessons to Indonesia’s unique context, the healthcare system can adopt more effective approaches and innovations.
Indonesia’s Battle Against Chronic Diseases: Conclusion
In combating non-communicable diseases (NCDs), collaboration, innovation, and training stand as pillars of progress. A united effort across sectors—healthcare providers, policymakers, private enterprises, and communities—is essential to creating impactful and sustainable solutions. Innovation, particularly in digital health technologies and data systems, bridges gaps in care and ensures efficiency in managing chronic conditions. Equally vital, continuous training equips healthcare professionals with the skills and knowledge needed for early detection, effective management, and patient-centered care. By prioritizing these interconnected strategies, Indonesia can not only reduce the burden of NCDs but also foster a healthier, more resilient society.
Empowering Healthcare Professionals to Combat Chronic Diseases in Indonesia
To further enhance the skills and knowledge of healthcare professionals in Indonesia, Zafyre offers eLearning training solutions with internationally and Ministry of Health certified courses. These courses aim to equip healthcare professionals with up-to-date information and effective techniques for preventing and managing chronic diseases. By enrolling in Zafyre’s training programs, healthcare professionals can stay updated with the latest advancements in healthcare and improve patient outcomes.
Join Zafyre today and be a part of the movement to combat chronic diseases in Indonesia.
Indonesia’s Battle Against Chronic Diseases: List of References
A. Indonesian Journal Articles
- Nurjanah, A., Sativa, S. Z., Astuti, A. D., Rangkuti, S. R., Nafisah, N., Fitri, N., Utami, R., & Nasution, I. S. (2024). Analisis kebijakan kesehatan mendorong partisipasi masyarakat dalam program pencegahan penyakit. Jurnal Anestesi: Jurnal Ilmu Kesehatan dan Kedokteran, 2(3), 178–191. https://doi.org/10.59680/anestesi.v2i3.1223
- Sitanggang, A. S., Imanuel, R. G., Rapa’, N. I., Shandie, W., & Halim, I. J. (2024). Telemedicine: Revolusi akses dan efisiensi pelayanan kesehatan di era digital. Nusantara Journal of Multidisciplinary Science, 2(1), 12–18. https://jurnal.intekom.id/index.php/njms
B. Other Journal Articles
- Arifin, H., Chou, K.-R., Ibrahim, K., Fitri, S. U. R., Pradipta, R. O., Rias, Y. A., Sitorus, N., Wiratama, B. S., Setiawan, A., Setyowati, S., Kuswanto, H., Mediarti, D., Rosnani, R., Sulistini, R., & Pahria, T. (2022). Analysis of Modifiable, Non-Modifiable, and Physiological Risk Factors of Non-Communicable Diseases in Indonesia: Evidence from the 2018 Indonesian Basic Health Research. Journal of Multidisciplinary Healthcare, 15(1), 2203–2221. https://doi.org/10.2147/JMDH.S382191
- Endarti, D., Andayani, T. M., Widayanti, A. W., Rohmah, S., Banjarani, R. R., & Ghearizky, N. A. (2024). Chronic disease costs from a patient’s perspective: A survey of patients with stroke, heart disease, and chronic kidney disease visiting a district hospital in Indonesia. Journal of Pharmacy & Pharmacognosy Research, 13(1), 274–283. https://doi.org/10.56499/jppres24.2036_13.1.274
- Malini, H., Efendi, F., Kadar, K., Putri Lenggogeni, D., & Puspita Sari, Y. (2023). Health literacy and associated factors among patients with chronic diseases in Indonesia. Journal of Public Health. https://doi.org/10.1007/s10389-023-02035-8
- Marthias, T., Anindya, K., Ng, N., McPake, B., Atun, R., Arfyanto, H., Hulse, E. S., Zhao, Y., Jusril, H., Pan, T., Ishida, M., & Lee, J. T. (2021). Impact of non-communicable disease multimorbidity on health service use, catastrophic health expenditure and productivity loss in Indonesia: a population-based panel data analysis study. BMJ Open, 11(2), e041870. https://doi.org/10.1136/bmjopen-2020-041870
- Mustika, R., Nishigori, H., Ronokusumo, S., & Scherpbier, A. (2019). The Odyssey of Medical Education in Indonesia. The Asia Pacific Scholar, 4(1), 4–8. https://doi.org/10.29060/taps.2019-4-1/gp1077
- Octavius, G. S., Wijayanto, R., & Yanto, T. A. (2023). Transformation of Indonesian Health System: The Impact on Medical Education. International Medical Education, 2(2), 96–99. https://doi.org/10.3390/ime2020009
C. Reports
- Karmini, N., & Alangkara, D. (2025, January 6). Indonesia launches free meals program to feed children and pregnant women to fight malnutrition. AP News. https://apnews.com/article/indonesia-prabowo-subianto-free-meals-children-mothers-213a04587203434f3f85950725e84a8b
- Putri. (2023, October 10). Opportunities and challenges for foreign doctors in Indonesia – Integrity Indonesia. Integrity Indonesia. https://www.integrity-indonesia.com/blog/2023/10/10/overcoming-medical-workforce-shortages-opportunities-and-challenges-for-foreign-doctors-in-indonesia/
- Reuters. (2024, July 10). Novo Nordisk, Indonesia’s Bio Farma sign deal to package insulin. Reuters. https://www.reuters.com/markets/deals/novo-nordisk-indonesias-bio-farma-sign-deal-produce-insulin-2024-07-10/
- Widianto, S. (2024, July 31). Indonesia raises smoking age limit, will curb cigarette advertising. Reuters. https://www.reuters.com/world/asia-pacific/indonesia-raises-smoking-age-limit-will-curb-cigarette-advertising-2024-07-31/
D. Other References
- Indonesian Health Economics Association (INAHEA). (2019). Economic impact of NCDs by health system perspective. Retrieved from https://www.inahea.org/wp-content/uploads/2019/11/Economic-impact-of-NCDs-by-health-system-perspective.pdf
- Sadomo, R., & Fauzi, L. (2021). Non-Communicable Diseases in Indonesia: Prevalence and Risk Factor. Proceedings of the 5th International Conference on Sports, Health, and Physical Education, ISMINA 2021, 28-29 April 2021, Semarang, Central Java, Indonesia. https://doi.org/10.4108/eai.28-4-2021.2312234
- Teplitskaya, L., Sucahya, P., Marbun, D., & Rakhmadi, M. (2021). Improving Planning, Implementation, and Monitoring of Minimum Service Standards for Health in Indonesia. In Health Policy Plus (HP+). http://www.healthpolicyplus.com/ns/pubs/18487-18881_IndoSPMBrief.pdf
- United Nations Population Fund (UNFPA). (2022). Policy-in-practice case study: Indonesia. https://asiapacific.unfpa.org/sites/default/files/pub-pdf/casestudy-indonesia_final.pdf
- United States Agency for International Development (USAID). (2020). Case Study: Opportunities for Increasing Youth Employment in Health in Indonesia. https://hrh2030program.org/wp-content/uploads/2020/08/TVET-Indonesia-case-study.pdf
- World Health Organization. (2019). Noncommunicable diseases country profiles: Indonesia. https://iris.who.int/bitstream/handle/10665/333799/NCD_CCS_2019_Country_Profile_IDN.pdf